July 26, 2022
As health care organizations adopt Collaborative Care, it is critical to standardize how both adoption and outcomes are reported in order to ensure accountability and growth. At Concert Health, we are proud to spearhead the development of rigor around Collaborative Care outcomes in our everyday efforts, and in our research alike.
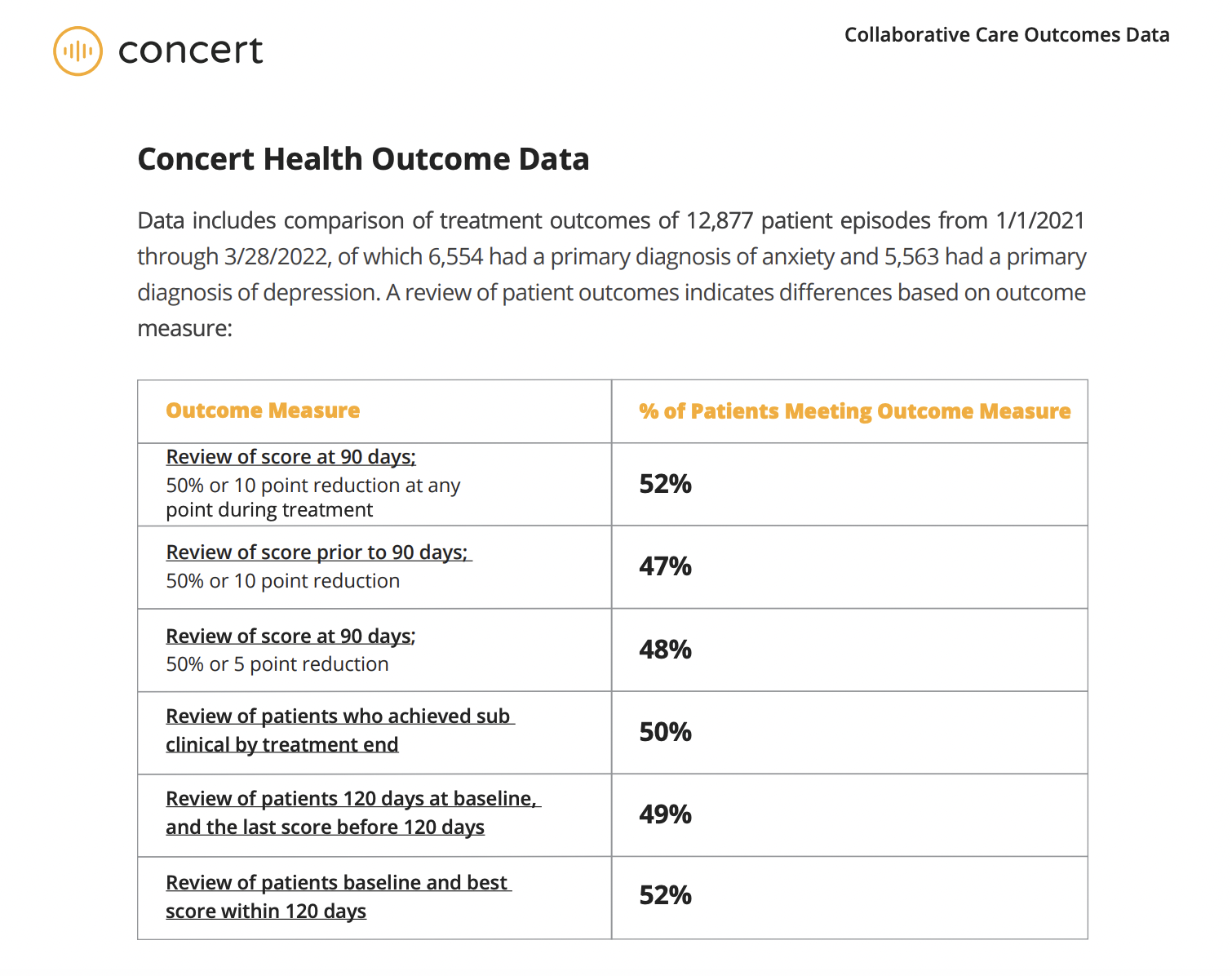
After studying 12,877 patient episodes, we learned a few things about how data is being collected across the board and came to some exciting conclusions about the work we are doing at Concert Health.
What is Collaborative Care?
Collaborative Care is an evidence-based model to identify and treat patients with depression and anxiety in health care settings. Since the introduction of Behavioral Health Integration billing codes in 2016, Collaborative Care has been rapidly adopted by health care settings nationally and on Medicaid fee schedules in almost half the states and nearly every commercial insurer in the country.
At its core, the Collaborative Care model is rooted in maintaining quality and is poised to overcome many of the obstacles that stand in the way of providing timely and appropriate behavioral health services, and evidence from our work at Concert shows just how dramatically this approach is improving patients’ lives.
Reporting Outcomes: Why the Inconsistency?
With the increase in adoption, comes the need for accountability, and as Collaborative Care has expanded, the reporting of outcomes and the methods to obtain them have been as varied as greatly as the organizations reporting them. That is where Concert Health comes in: we have sought to spearhead the development of rigor around Collaborative Care outcomes and bring results into the light.
In a recent STAT health tech newsletter, reporter Mario Aguilar put it this way:
“You wouldn’t compare a measurement in kilometers to a measurement in miles, but in a new paper, Concert Health argues something very similar is happening among the crop of new companies offering collaborative care to treat behavioral health issues in primary care. Concert says that companies reporting their results aren’t all using the same treatment windows or targets. Concert offered up its own scores to show how the most rigorous form of measurement can impact how effective a treatment looks. (Spoiler: Concert thinks it’s very rigorous.)
As our co-founder Virna Little told STAT, the goal is to encourage consistency and transparency: “If you’re going to be in this space, and you’re going to say you’re getting people better, let’s talk [about] what your outcomes are,” she said.
Collaborative Care Outcomes Data
While it is helpful to look at outcome measures through a variety of “lenses,” the ability to have consistency in reporting Collaborative Care outcomes will help to identify best practices, and the ability to contribute to best practices will expand overall learning and the adoption of the model on a national scale, leading to increased access and better outcomes.
Dedicated to raising the bar through consistency and rigor, we have published a Collaborative Care Outcomes Data report, in which we offer up our own scores to demonstrate how the most rigorous form of measurement can impact how effective treatment looks. Read more here.